TMJ is short for the TemporoMandibular Joint (jaw joint). TMD stands for TemporoMandibular Dysfunction. TMJ and TMD have been used synonymously to refer to a number of craniofacial problems and pains associated with the temporomandibular joint. The temporomandibular joints are located on either side of the face and connect the lower jaw to the skull. They are the most unique and complex joints in the entire body.
what is tmj / tmd ?
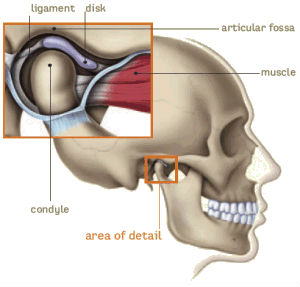
The TM joints work in synergy with the facial bones and multiple pairs of muscles to allow opening and closing of the mouth, chewing, swallowing and speech, as well as to enable the forward, backward, rotational, and side-to-side movements of the lower jaw.
Any disturbance to the perfect facial balance can trigger the cycle characteristic of TMJ disorders, which affects muscles and joints on all areas of the face, neck, and back. When muscles and joints are not working together correctly, muscle spasm can result which produces pain and dysfunction. Due to this complex system, a problem in one area can cause symptoms elsewhere.
In a normal joint, the disc, a thin piece of cartilage, acts as a cushion or shock absorber between the condyle and the glenoid fossa. It is held in place and guided by muscles and ligaments. When the lower jaw opens and closes, the disc stays between the condyle and the glenoid fossa at all times.
The following are contributing factors to TMJ disorder: trauma to the head and face, whiplash, uneven bite (malocclusion), bruxism (grinding your teeth), clenching etc. When trauma to the TM joints is prolonged, the body begins to compensate by involving muscles in other areas: the face, neck, throat, upper and lower back, arms, etc.
TMD is often a chronic and degenerative disease. Anyone experiencing headaches, earaches, dizziness and clicking or popping in the jaw joints should schedule an appointment for a thorough examination with a qualified dental professional, before their symptoms become more severe.
signs and symptoms
TMJ disorders have been called the “Great Impostors” because many of the symptoms have overlapping characteristics, which often mimic other conditions. Indeed, it is quite common for people to seek the care of a medical doctor or medical specialist in search of a cure or answer. Most, however, never think to contact a dentist trained in TMD since the symptoms are primarily medical in nature.
Do you suffer from any of these? (Click the symptoms for more information)
causes
According to statistics published in the Journal of the American Dental Association in 1990,* 44% to 99% of TMJ problems are caused by trauma. By trauma, we mean an injury as obvious as a blow to the jaw with a fist or something as subtle as a whiplash injury, with or without direct trauma to the head or jaw. (*JADA 1990;120:267) An overwhelming majority of patients who sustain whiplash injuries in motor vehicle accidents (MVA) also dislocated one or both temporomandibular joints at the same time without having impacted their face or head against the steering wheel, door column, windshield or other parts of the car.
Some of the causes of TMD include:
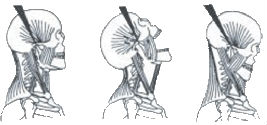
Whiplash injury and automobile accidents
Whiplash typically occurs when the head is thrown backward and forward while riding in a car that is hit from behind or the side. Extensive research shows that most flexion-extension injuries occur following what is called “minor head injuries.” This means that it is not necessary to suffer a fracture or even a direct head impact. In fact, most patients report that their head was simply snapped backward and forward or side-to-side. This motion causes damage to the muscles and ligaments, which support the jaw joint. When these muscles and ligaments are injured, this can cause an anterior displacement of the protective disc and result in a dislocated jaw joint on one or both sides.
Intubation procedures in hospitals
Patients that undergo surgical procedures with general anesthetic are usually intubated through the mouth. Intubation involves placing a tube down the throat to keep the airway open during surgical procedures. Occasionally, the jaw can be dislocated during this procedure due to the forced opening of the mouth and the hyperextension of the ligaments and tissues while inserting the tube. Some patients may experience clicking in the jaw, limited opening of the mouth, facial pain, and headaches post surgically. Those patients who have already been diagnosed with a TM disorder should advise the anesthesiologist that they wish to be intubated through the nose during any surgical procedure to prevent further damage to the joint and its surrounding structures.
Trauma to the head, face or jaw
A severe blow to the head or to the jaw can cause the disc to be dislocated due to the force of the impact. Patients may experience swelling, limited opening and clicking in the joint. Patients with this acute injury should seek emergency treatment immediately to avoid further damage to the joint.
Regardless of the type of trauma sustained, the temporomandibular joint is affected like no other joint in the body. Behind the condyle, there are several structures that affect the health of the jaw joint itself. One is the posterior ligament, which acts as a rubber band to pull the disc backward during closing of the jaw. Like all joints, the TM joints contain a large amount of nerves and blood vessels which, on a subconscious level give the brain information about the position and condition of the joint. When the mouth is closed, the disc, which has no feeling, acts as a shock absorber to prevent the nerves and blood vessels from being compressed. When the mouth opens and the condyle and the disc move forward, the blood vessels expand to fill the vacated space. When the condyle is pushed too far backwards in the joint, it can slip off the cartilage disc and impinge onto these nerves and blood vessels. Once these are compressed, the whole structure is unbalanced, affecting the nerves, the ligaments and the muscles of the head, neck and face. This dislocated jaw causes pain and other symptoms affecting a person’s health and quality of life.
diagnosis
TMD diagnosis is a complex and often daunting process. This explains why physicians and dentists who are not board-certified orofacial and craniofacial pain specialists may miss a potential TMJ disorder in a patient that is suffering from chronic head, neck and/or facial pain.
How is the diagnosis made?
The usual evaluation of the TMJ involves a physical examination of the muscles of the head, face, neck and shoulder with manual palpation. The doctor feels for muscle spasm and rules out “trigger points” which can refer pain to other areas. Ranges of Motion Studies–measurements of jaw movement when moving side to side and on full opening of the mouth, are assessed. General skeletal alignment is also assessed. Additionally, radiographs allow us to see actual pictures of the joint components and their relative state of health. In many cases, additional tests may be recommended. At our office we also utilize the latest in computer diagnostics to measure and record jaw joint activity and jaw movement.
Computerized Diagnostics
We use the latest in computerized diagnostic modalities including EMG (electromyography), ENG (Electrognathology-Jaw Tracking) and JVA (Joint Vibration Analysis). The use of EMG, ENG and JVA along with radiographs allows for a more accurate determination of the nature or type of TMD experienced.

JVA (JOINT VIBRATION-NOISES ANALYSIS)
Joint Vibrationa Analysis is a device that measures how well the joint functions while in motion. This is accomplished by placing headphones over the joints and recording the vibrations(noises) of either soft tissue (quiet, when disc is working properly) or bone on bone grinding (crepitus, gravel sounding).

ENG / JT (Jaw tracking)
Jaw Tracking (Electrognathography) is used to track the jaw movements three dimensionally and to record the point of dysfunction so it can be corrected. A headset is placed on the patient and with a magnet inside their lower front teeth, a recording of the lower jaw movement is made. With this diagnostic tool we can measure and analyze jaw movement during clenching,chewing and swallowing. Jaw tracking is a completely non-invasive technique.
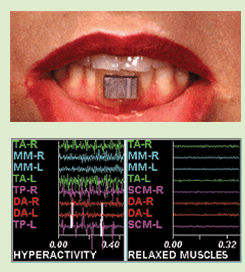
Emg (Electroomygraphy)
EMG is a non-invasive device used to evaluate muscle activity through surface/skin electrodes

Radiographs (X-Rays)
TMJ x-rays are important to determine the position of the condyles (top of the lower jaw bone).
